Health Plan of San Joaquin/Mountain Valley Health Plan (“Health Plan”) contracts with external individuals and organizations to provide efficient and cost-effective Medi-Cal services to our members. Some of these services are Benefits and Administrative Functions that Heath Plan itself must perform. These individuals and organizations are known as delegates.
Delegates must not subdelegate the performance of any Benefits and Administrative Functions to another individual or organization without the express written consent of Health Plan and the Department of Health Care Services (DHCS). If sub-delegation is authorized, delegates agree to monitor and oversee their subcontractors’ performance of sub-delegated functions.
Delegates and their subdelegates are required to comply with Health Plan’s policies and procedures and are required to follow the same Federal and State rules and regulations that Health Plan is required to follow.
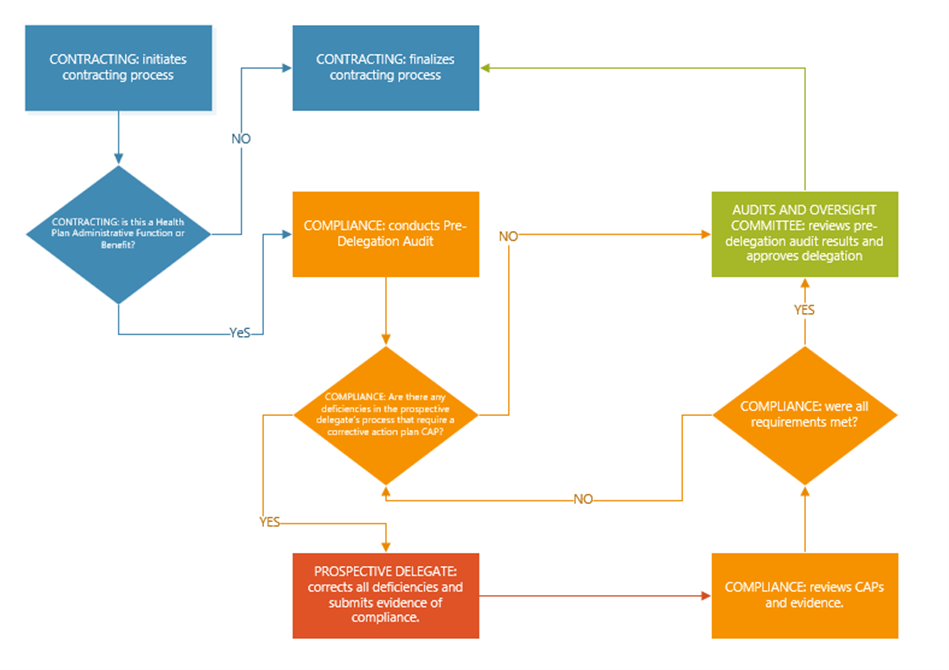
Prior to contracting with a delegate, Health Plan conducts a pre-delegation audit. This audit is intended to evaluate a prospective delegate’s administrative capacity, task expertise, and budgetary resources to perform Health Plan Administrative Function or to administer a Medi-Cal Benefit. Once a pre-delegation audit is completed, Health Plan will implement a contract with the delegate.
Pre-Delegation Audit High-Level Process
Health Plan does not delegate the responsibility of processing member appeals and grievances.
Delegates must be able to demonstrate that they have the staffing, information systems, policies, procedures, tracking and reporting mechanisms that are needed to perform the functions that are being delegated. Delegates must also demonstrate that they can perform other activities that impact the performance of delegated functions. For example: an individual or organization delegated to perform case management must have systems (information systems, process, staff, etc.) in place to also protect Health Plan’s members’ health information. Delegates’ staff must also have the required education, licensures, work experience, etc. to perform the delegated functions. Finally, Delegates’ must have and maintain their ability to generate the cash flow necessary to meet ongoing operational expenses and debt repayments.
Health Plan continually assesses delegates’ ability to perform delegated functions through ongoing monitoring, annual performance audits, and analysis of data. Delegates must cooperate, participate, and comply with Health Plan’s and DHCS’ audit and monitoring activities. In addition to evaluating how delegates perform delegated functions, Health Plan also conducts oversight of the following non-delegated activities that are essential for the delivery of their contractual obligations with Health Plan:
- Financial Viability
- Fraud, Waste, and Abuse
- HIPAA Privacy and Security
- Ownership and Control Disclosure
Health Plan will require delegates to develop and submit a corrective action plan(s) (CAP) when deficiencies or non-compliance with Medi-Cal requirements is identified through any of Health Plan’s oversight activities. Delegates will create and, upon approval by Health Plan, implement such CAP(s). Health Plan will monitor delegates’ ongoing performance to ensure corrective actions take place in a timely manner, and will perform additional follow up audits, as necessary, to verify the completion of CAP(s). Health Plan has the right to directly monitor and oversee delegates’ subcontractor’s performance of sub-delegated functions by conducting continuous monitoring and an annual oversight audit as necessary. Below is a list of Health Plan audits and oversight policies and procedures:
- Delegation of Administrative Functions (CMP36)
- Oversight of Delegated Administrative Functions (CMP31)
- Financial Oversight of Third Parties (CMP33)
- Corrective Action and Sanctions (CMP34)
- Annual Subnetwork Certification (CMP47)
Health Plan communicates changes to current or new regulations and requirements as soon as they become available. Delegates must comply with changes or new requirements within 30 calendar days of their effective date. This information is communicated via the Provider Manual, Provider Alerts, and targeted correspondence.